Pretesting Indwelling Urinary Catheter Balloons
The insertion of indwelling catheters, also known as retention catheters, is a medical procedure frequently employed during hospitalization. It’s a common procedure especially in acute settings, in various types of health-care units (nursing homes, emergency units, palliative care units etc.) In these scenarios, depending on the type of health care provided, around 20 to 30 percent of patients will require catheterization at some point during their care.
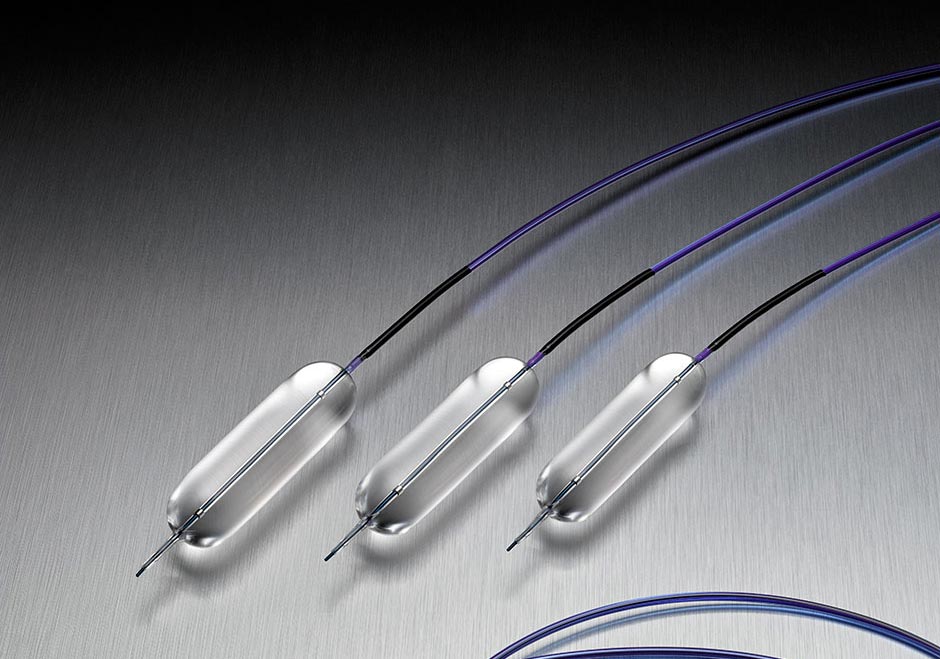
Indwelling catheters, as their name implies, are inserted in the urethra to facilitate the evacuation of urine. Because they are invasive devices, urinary tract infections are quite common, affecting a patient’s comfort and safety.
Historically, in order to avoid infections, catheter malfunction or various production errors, nurses pretested indwelling catheters before insertion. This practice, although very common during up until the 1970s, quickly became redundant thanks to the availability of single-use sterile catheters. Today, virtually all manufacturers pretest indwelling catheters before packaging, so every catheter is fully functional. Moreover, almost all manufacturers specify that catheter pretesting should not be done because it can damage the physical characteristics of the device.
Let’s take a look at what the medical evidence has to say about this contradictory subject. Should you pretest indwelling catheters or not?
Virtually all evidence-based practice (EBP) recommendations don’t support the pretesting of indwelling catheter balloons. This refers to the practice of inserting sterile water through a syringe inside the catheter to test its physical attributes. The rationale behind this recommendation is that, when testing the indwelling catheter, the liquid used may stretch, tear and distort the catheter, resulting in irreparable damage to the rubber material. This can lead to pain or trauma for the patient during insertion, which can further cause additional medical issues.
Although in the past, testing was required to test whether a catheter was defective or not before use, modern catheters do not require this procedure. Even historically, pretesting didn’t guarantee that the balloon was not defective and would work properly once inserted. What’s more, pretesting silicone or latex catheters is not recommended, as it can cause ruptures or tears which can hurt the inner parts of the urethra. The sterile package which includes the catheter generally has clear instructions regarding balloon pretesting. The general consensus is to avoid testing of catheters at all costs.
Catheter insertion should be done carefully to avoid causing harm to patients. To make sure you follow procedures during handling and insertion, review your facility’s guidelines on catheter insertion or pretesting. Generally, all hospitals or health-care units have strict rules and guidelines on how should catheters be handled, used or whether pretesting is allowed. All approved nursing manuals nix pretesting of indwelling balloon catheters entirely, so nurses entering the workforce are not taught this procedure at all.
Additionally, CDC’s guidelines (Center for Disease Control and Prevention) recommend health-care personnel who use catheters or take part in the catheterization procedure to follow continuous training in order to master the correct use of the devices. The training also helps personnel avoid various possible complication of urinary catheterization, such as urinary tract infections, urosepsis or other related medical conditions.
Conclusion:
Nurses are responsible for keeping up with the EBP recommendations as well as the regulations in the hospital environment. They are obligated to know the proper catheter insertion procedures, understand the risks and benefits of the procedure and how to avoid harming the patients. Continuous training and supervision helps nurses develop consistency in these highly standardized medical procedures.